Local lives filled with risk have gotten a lot riskier lately. In the Cowichan region, the COVID-19 pandemic is a triple whammy for people who use drugs and don’t have secure housing.
Already dealing with the opioid overdose crisis and the affordable housing crisis, they are particularly vulnerable to contracting the coronavirus. They can’t stay home, and access to food, shelter and services has been reduced. Those taking medications often need to see a pharmacist every day. Those using street drugs often depend on daily (or more) contact with dealers.
Two weeks ago, Dr. Elizabeth Plant, an addiction physician who treats patients through Duncan Mental Health and Addiction Services and the Cowichan District Hospital, told me that she is terrified about the potential of COVID-19 spreading very rapidly among people living on the streets. “It’s going to be devastating,” she said.
But when I spoke again with Plant earlier this week, there was a bit less anxiety in her voice. She told me that there may be a silver lining to this disaster. In light of the gravity and urgency of this threat, there’s new momentum on evidence-backed solutions to keep people on the streets safer and healthier.
Safety in numbers
On the streets, there’s safety in numbers. “Staying close to one another is paramount to maintain their safety on the streets and it is unthinkable to ask people in such a precarious situation (and with no additional support) to isolate themselves,” wrote frontline workers on Vancouver’s Downtown Eastside in an open letter to government officials.
Not everyone who lives on the streets uses illicit drugs. But those who do face additional risks. Already, the toxic and unreliable supply of drugs on the streets is killing people. At least 75 people have died from overdose in the Duncan area since 2016, Dr. Shannon Waters, medical health officer for the Cowichan Valley region, told me earlier this year. When people use drugs alone, there’s no one to administer naloxone or call for help.
“We can’t isolate ourselves because we die,” Emma Nunn tells me. Nunn says she is homeless and addicted to heroin, and spoke to me last week about how people on the streets are coping with COVID-19. As borders close and travel is restricted due to COVID-19, Nunn says that the word on the street is that the supply of heroin is drying up in Cowichan. Health experts fear that this will make the street drug supply even more toxic than it already is.
Mounting calls for safe supply
For the past couple of months, I’ve been looking into how the opioid overdose crisis is playing out on the streets of Duncan. When I ask service providers, local officials, people who use drugs and local business owners what can be done to improve the situation, the solution that comes up most often is to make legal, regulated drugs more available.
This is known as safe supply. Advocates claim that it’s a win-win for people who use drugs and the overall community. By cutting toxic street drugs out of the equation, safe supply can greatly reduce overdose deaths as well as the need for people who use drugs to resort to illegal activities such as shoplifting, prostitution and drug dealing to afford their habit. There’s evidence from early safe supply pilots that it can help those who are resistant to other available treatments.
Illicit drug use is common in Canada, across all walks of life. Most overdose deaths in B.C. occur in private residences.
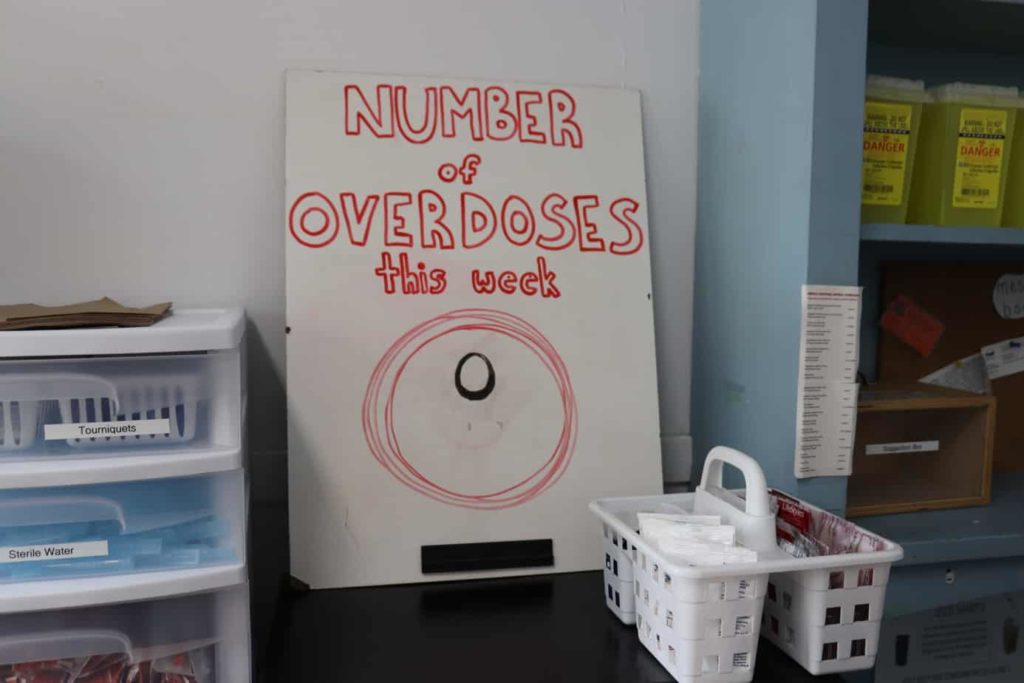
As of early March, about 100 to 180 people each day were using drugs at the Overdose Protection Site in Duncan, according to Melissa Middlemiss, manager of human resiliency programs at the Cowichan Valley branch of the Canadian Mental Health Association. The OPS is a harm reduction site where people can go to use drugs and trained staff are available to assist in the event of an overdose.
Supervised drug use saves lives. Staff at the facility intervened in 170 overdoses last year, and no one died. But people must bring their own drugs to the facility. And those drugs remain highly toxic because of the strong and unpredictable street supply.
The Cowichan Leadership Group, with representation from local elected leaders, Island Health and the RCMP, recently pushed the province for a safe supply pilot project here. B.C. denied the funding.
As a result, it didn’t appear, in the pre-COVID-19 world, that safe supply was going to happen anytime soon.
The tide turns
But the pandemic changed all that. Last Thursday, the province released guidelines from the BC Centre on Substance Use that allow physicians, on an interim basis, to prescribe a safe supply of drugs, including opioids like hydromorphone, to people who meet certain criteria.

This is wonderful news, says Plant. “I’m so glad because there is no way we can expect folks with active substance use disorders to be able to successfully socially isolate or to be able to survive in a state where the supply is going to be even less reliable.”
Federal exceptions announced earlier this month to the Controlled Drugs and Substances Act have made safe supply more broadly available in B.C. These exceptions will be in effect until September 30, although there is the possibility that they will be extended. Provincial PharmaCare will cover the costs of providing safe prescription drugs to people who meet the criteria.
To qualify, people need to have a history of ongoing active substance use, have a high risk of withdrawal or overdose, and be at risk of COVID-19 infection or have a confirmed or suspected case. People can ask their doctors about it or get assessed at a rapid access addiction clinic.
The prescription medications will be in oral doses and dispensed to individuals on a daily basis, to prevent people from taking too much or reselling the drugs, Plant says.
Even with prescription opioids, it’s important that people use with a buddy, Plant says. The BC Centre for Disease Control has also released guidelines for safer drug use during the COVID-19 pandemic.
New protocols for methadone treatment
The pandemic also complicates the delivery of medications, including methadone and others, for people on opioid agonist therapy. OAT refers to the prescription of slow-acting opioids, which can keep withdrawal at bay and help people with opioid use disorder function in daily life. Current programs often require people to show up to a clinic daily and take medication under supervision. “Going into a pharmacy every day as a person who’s in a high risk population of contracting the virus and spreading the virus is not ideal,” Plant says.
In response to these concerns, the province has granted new powers to pharmacists. They are now able to take verbal orders for opioids from doctors, continue a prescription without doctor approval for patients about to run out of their supplies, and directly transfer prescriptions to other pharmacists.
“It gives the pharmacist more power and flexibility to be able to make sure that people’s prescription of OAT is seamless in this time,” Plant says.
Another notable change is around “carries,” the term for takeout doses. New protocols developed by the BC Centre on Substance Use allow doctors more discretion to prescribe more medication for patients to take with them. Plant notes that patients who lack housing often don’t have a place to safely store OAT medicines. She says that during this time of crisis clinicians must weigh whether the risk of having patients go to the pharmacy every day is greater than risks of overdose and other potential harms from dispensing a larger quantity of medication.
Shelter is critical
Improved access to treatment isn’t enough, Plant says. Many people with substance use disorders also need shelter to stay safe through this crisis. Cowichan’s COVID-19 Task Force for Vulnerable Populations announced on April 1 that it has submitted a 30-day emergency plan to BC Housing and Emergency Management BC to house, feed and support people who need it.
There are plans in the works to deliver medications to the emergency shelters daily, to limit the risks of dispensing larger quantities, Plant says. She notes that while her work is very challenging right now, it is an exciting time to be working in addiction medicine.
“One of the silver linings of something really terrible is that all of these things which would have taken years to move forward on are given the light to go ahead now,” Plant says. If there’s evidence that these interventions help, it’s more likely they’ll continue beyond this crisis. “Once you put something in place, it’s really hard to peel it back.”
Resources:
Some of the following resources were culled from an information sheet prepared by the Cowichan Community Action Team:
- Opioid Agonist Therapy is accessible from the Phoenix Wellness Centre (604-260-7252) or Canada Avenue Clinic (250-597-1184).
- For safe supply, reach out to your doctor or the Rapid Access Addiction Clinic in Victoria (250-519-3485).
- The Overdose Prevention Site in Duncan remains open at this time, with increased sanitation and precautions.
- Naloxone is available locally at: Margaret Moss Health Unit, CMHA Festubert, OPS Duncan, Phoenix Wellness Clinic, Cowichan District Hospital, Duncan Mental Health & Substance Use Services, Ladysmith Community Health Centre, Lady Minto Hospital (Salt Spring Island).
- Towards the Heart provides information on recognizing signs of different types of overdose (opioid, amphetamines, alcohol) and on harm reduction strategies.
- The BC Centre for Disease Control has produced an information sheet on harm reduction and overdose response during COVID-19. [end]